Those of us who stay on top of patient advocacy-related news got a jolt from this headline, “Patient Advocacy Groups Rake In Donations From Pharma.” Just the jolt itself suggests that a few clarifications need to be made about our work as independent, private patient advocates.
This is a topic I have written about several times in the past, but because it has big ripple effects, and because some of the people you connect with may be confused, you’ll need to clarify for them, so it bears repeating.
It’s about allegiance. And it’s classified in the same sphere of conversations and objections as these:
But the hospital has a patient advocate and I can talk to her for free. So why should I pay you?
I got a flyer in the mail from my insurance company and they offered a patient advocate to help me for free! So why should I pay you?
Anyone who has begun marketing a private advocacy practice has heard these sorts of objections. Like all roadblocks found in the healthcare system, I’m going to suggest you walk through the right answers with them, because it applies in all cases.
This is the way to overcome their objections.
You Get What You Pay For
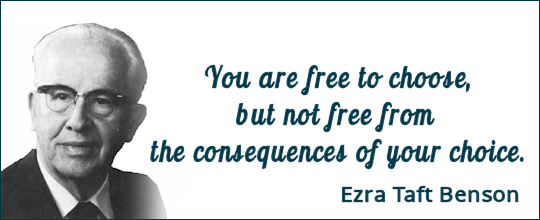
The hospital advocate’s allegiance is to…. the hospital. That’s who pays her. While there may be many things she can accomplish for a patient or caregiver, at the end of the day, her real job is to keep the hospital out of hot water. In most cases (95+%) she works for the Risk Management (legal) department of the hospital, and her hospital allegiance will only allow her to go so far to help a patient or caregiver.
So ask, “What are the consequences of tapping into the hospital-paid advocate?” An independent, private advocate has no such constraints.
Fairly new on the landscape is the insurance company employed advocate – the one on the other end of the phone (“Ask a nurse!”). And yes, that’s who pays her. But remember, the goal of the insurance company is to make as much money as it can, which it does by denying care. While there may be some things the insurance advocate can help with, at the end of the day, her job is to be sure the insurance company doesn’t pay one cent more than it has to for its customer’s care. So the question is – do you want the people who won’t pay for your care advising you on what care you need? Do you trust them to suggest the real treatment that may be necessary or preferred if it happens to be more expensive?
So ask, “What are the consequences of tapping into the insurance company-paid advocate?” An independent, private advocate has no such constraints.
The article mentioned at the beginning of the post refers to “patient advocacy groups”… But they aren’t us either. They are groups like the American Cancer Society, or the Alzheimers Association, or any of the disease or condition-specific advocacy groups. What keeps them afloat? Individual donations are usually just a small percentage of their income. It’s the drug companies that donate the most – in trade for making sure their drugs are front and center in all discussions about treatment. The worst part is that there is almost no transparency among these advocacy groups. In order to figure out where their drug money comes from, you often have to see who leads their board of directors. (And that’s what that article cited above, linked below is about.)
So ask, “What are the consequences of tapping into the disease/condition fundraiser advocacy groups?” An independent, private advocate has no such expectations to deal with.
The real problem here is that there are many approaches to advocating and assisting people who are forced to tap into the healthcare system. But the healthcare system is set up to suck as much money as it can from all of those people. Thus, when the term “patient advocate” or “health advocate” is aligned with them, there is bound to be confusion.
So – what can we private, independent advocates do about that? How can we distinguish ourselves, and overcome objections?
The best answer is to be VERY CLEAR on allegiance – front and center. Make sure allegiance is part of your discussion about your work with anyone new: a prospective client (of course), but also a friend who is just hearing about your advocacy for the first time, a neighbor, your pastor, priest, or rabbi, your brother-in-law, the man standing next to you at the check-out counter – everyone.
Make sure you invoke, ‘You get what you pay for, so you have to know who’s doing the paying.” Then discuss the consequences of getting help for “free.”
Don’t stop at, “I’m starting (or building) a patient advocacy practice.” Instead, elaborate a little, “My practice is focused only on the person I’m working for. I’m not being paid by a hospital, or an insurer, or pharmaceutical company money. Since the patient or his loved one pays me, my allegiance is 100% focused on his needs.”
Because they’re not us. And we’re not them. And yes, the difference means paying the consequences.
- Patient Advocacy Groups Rake In Donations From Pharma (article cited in the first paragraph, above)
- An Advocate’s Allegiance Makes All the Difference
- Patient Advocacy and the Allegiance Factor
- Like Putting Ponze in Charge of My Retirement Savings – a Rant
LEARN ABOUT APHA MEMBERSHIP | FIND MORE REASONS PATIENTS NEED ADVOCATES



Trisha,
Thank you for highlighting such a clear and straightforward way for advocates to address this issue. Discussing the Allegiance Factor AND the issues of ?transparency? are 2 excellent ways to begin educating others who become ?enchanted? by the offer of a ?free? patient advocate.
Melonie Britton BA, BScN.
Yes- Thank you Trisha. Allegiance. We pledge it to each person who becomes our client. (And hopefully to all others in our lives)
Kathy King
Marin Healthcare Navigation